ACL Tear Surgical Repair in Indianapolis, IN and Mooresville, IN
ACL Reconstruction (Quadriceps Autograft)
Anterior Cruciate Ligament (ACL) Tear and Reconstruction with Quadriceps Autograft
Non-operative treatment:
Not all ACL injuries require surgery. Some patients are able to recover with rehabilitation, bracing, and modification of activities. This treatment is reserved for older patients or patients who do not want to go back to higher-intensity sporting activities. You are able to run in straight lines, play golf, and swim without an ACL.
Operative treatment:
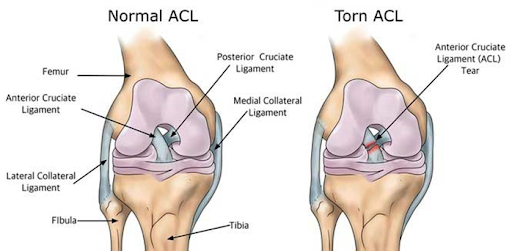
For patients who want to get back to sporting activities that include cutting and pivoting, ligament reconstruction is the treatment of choice. When the ACL tears, its torn ends are like a wet mop. Because of this, the torn ligament cannot be sewn back together (repaired). ACL reconstruction involves replacing the torn ACL with part of a tendon taken from another area of your body. The goal of knee ligament reconstruction is to tighten the knee joint and restore its stability. It helps you avoid further injury, and works to prevent arthritis long-term. The procedure is performed under general anesthesia, and a nerve block is normally given pre-operatively to help with pain after surgery.
The knee is first examined with an arthroscope, a small video camera, inside the knee to assess the ACL and additional structures that may have been injured. During this part of the procedure, other injuries will be addressed (meniscal tear, cartilage injury, scar tissue clean-up, etc.).
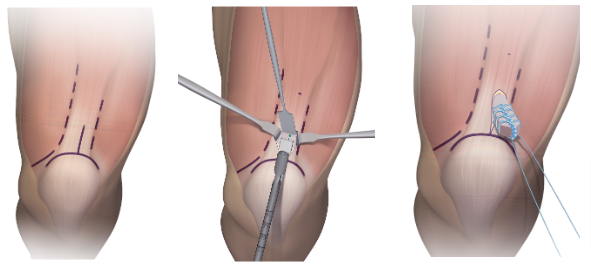
A tissue graft is then harvested from the quadriceps tendon. The quadriceps tendon connects the large muscle of the thigh (quadriceps) to the knee cap (patella). For the quadriceps tendon graft, a 1-2” incision is made over the top of the knee cap and a small sliver of the quadriceps tendon is removed. The remaining quadriceps tendon on either side of the graft is sutured (stitched) back after its removal.
Anterior Cruciate Ligament (ACL) Tear and Reconstruction with Allograft Tissue
Not all ACL injuries require surgery. Some patients are able to recover with rehabilitation, bracing, and modification of activities. This treatment is reserved for older patients or patients who do not want to go back to higher-intensity sporting activities. You are able to run in straight lines, play golf, and swim without an ACL.
Operative treatment:
For patients who want to get back to sporting activities that include cutting and pivoting, ligament reconstruction is the treatment of choice. When the ACL tears, its torn ends are like a wet mop. Because of this, the torn ligament cannot be sewn back together (repaired). ACL reconstruction involves replacing the torn ACL with part of a tendon taken from another area of your, or someone else’s, body. In patients who are over 35 years old or have lower physical demands, a cadaver graft may be used for the reconstruction to minimize the amount of morbidity (injury, pain) that occurs when taking a tendon from the patient’s own body. Techniques today are much improved for obtaining and cleaning cadaver tissue, so these allografts can recreate a strong, durable ligament and be done in a safe manner.
The goal of knee ligament reconstruction is to tighten the knee joint and restore its stability. It helps you avoid further injury, and works to prevent arthritis long-term. The procedure is performed under general anesthesia, and a nerve block is normally given pre-operatively to help with pain after surgery.
The knee is first examined with an arthroscope, a small video camera, inside the knee to assess the ACL and other structures that may have been injured. During this part of the procedure, other injuries will be addressed (meniscal tear, cartilage injury, scar tissue clean-up, etc).
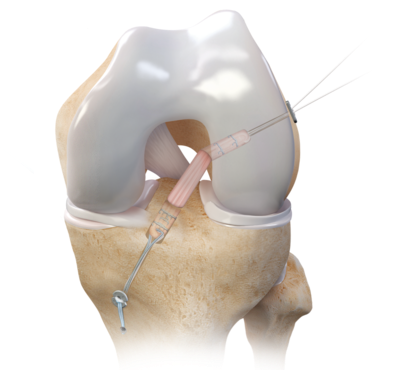
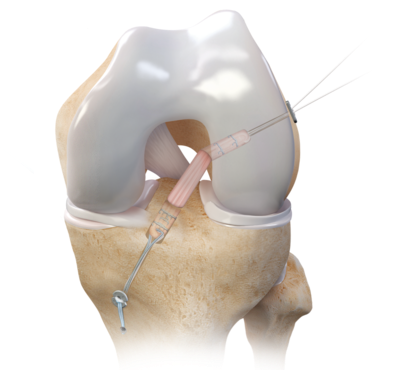
An allograft tissue graft (cadaver tendon and bone) is used. Small holes are drilled into the upper (femur) and lower (tibia) leg bones around the knee joint. These holes form tunnels in your bone to put the graft. The graft is then pulled into the holes in the tibia and femur. The new tendon is then fixed into place with metal buttons. The wounds are then closed with sutures. If a meniscal repair is performed, you will be placed into a brace that is locked in extension (straight). If only an ACL reconstruction is performed, you will not need a brace after surgery.
Revision Anterior Cruciate Ligament (ACL) Reconstruction
ACL reconstruction surgery is very effective, but some patients may experience a re-tear of the new ligament as a result of a recurrent injury or gradual stretching of the graft over time. In these cases, a revision ACL reconstruction is typically recommended. Patients may also experience a re-tear from new knee trauma, returning to athletic activities too soon, failure to wear the brace or follow rehabilitation guidelines following surgery. When a re-tear occurs, the knee must be examined and imaging (such as x-ray, MRI, CT scan) will be needed to determine the cause.
Graft choice: for primary (first-time) and revision ACL reconstructions in active patients, I prefer to use the quadriceps tendon. In patients who are slightly older or less active, an allograft (cadaver) may be used. In the rare case that the quadriceps tendon has already been used for a prior ACL surgery, my graft of choice is the contralateral (opposite leg) quadriceps tendon.

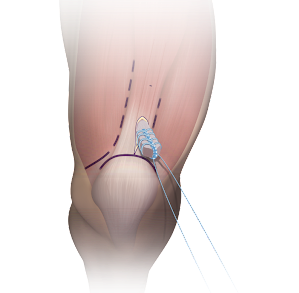
Lateral Extra-Articular Tenodesis (LET): in revision ACL reconstructions, there is oftentimes increased laxity (movement) of the knee. This laxity may also be present in patients with a first-time ACL tear. Examples of this increased laxity are patients who are able to hyper-extend the knee or have a very unstable knee after their first injury. In the above circumstances, a strip of the iliotibial (IT) band is placed into a tunnel in the femur (thigh bone) to prevent the increased rotation of the knee that is associated with injuries to the ACL. This is performed through an incision over the lateral (outside) of the knee and is done at the same time as the ACL reconstruction. With an LET, you will be in a brace for 6 weeks. Otherwise, the post-operative recovery is the same.
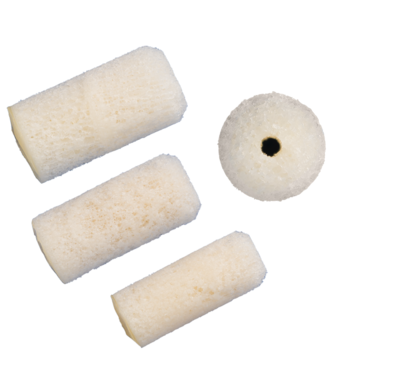
Bone grafting: a two part surgery may be necessary following a failed ACL reconstruction. Patients who have wide bone tunnels, tunnels in nontraditional positions, or poor bone quality, typically benefit most from a staged procedure. First, a bone grafting procedure designed to fill in the holes with new bone is performed. Then approximately four to six months later, a revision ACL reconstruction with a new graft will be performed.

Hardware removal: if screws are in the way of drilling new tunnels in the bone, they may be removed. This could involve an extra small incision, but most of the time can be done through the incisions made for the ACL reconstruction. If the screws are not in the way, they are normally left in place and do not cause any harm.
Tibial Spine (Eminence) Fracture
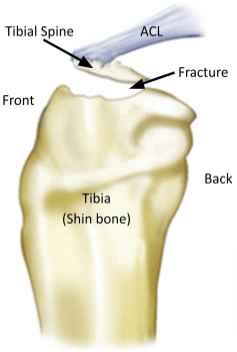
Tibial spine fractures are relatively uncommon injuries. Frequently these injuries occur during sports, and have classically been associated with a hyperextension (knee straightens too much) injury. They are most common in children and adolescents who are still growing, usually between ages 8-14. During this time of growth, the ligaments (like the ACL) can be stronger than the bone (like the tibial spine). The injury creates pulling along the ACL and causes an avulsion (breaking off) of the tibial spine. In adults with a similar injury pattern, the ACL is more often torn.
Non-operative treatment:
If the piece of bone that is fractured is not displaced (more of a crack in the bone) or barely displaced, treatment is usually casting or a brace to allow the bone to heal on its own. Frequent follow-up x-rays are necessary to make sure the bone does not move over time.
Operative treatment:
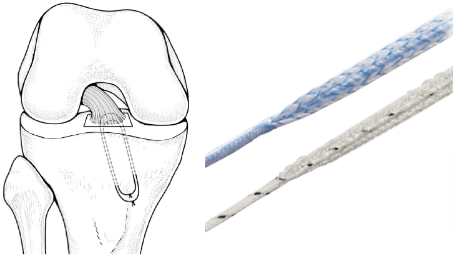
If the fracture is displaced (pulled away from the underlying tibia), surgery is required to get the bone to heal appropriately. Since the ACL attaches to the bone, healing is very important to regain stability of the knee. Surgery is usually arthroscopic (minimally-invasive) with a camera and specialized instruments to put the bone back to the correct position. A large piece of suture (much like a shoe string) is passed through the broken fragment and then secured down to the tibia (shin bone) with a small metal button. This surgery is outpatient (go home the same day) and performed under general anesthesia. You will be placed in a brace locked in extension (straight-leg) after surgery and you will be unable to put weight on the leg for at least the first week.
