Patellofemoral
Patellofemoral Syndrome Treatment in Indianapolis, IN and Mooresville, IN
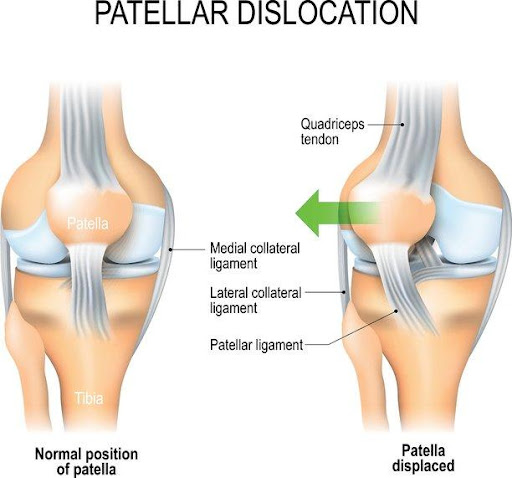
Patellar Instability / Dislocation

Patellar dislocations can cause injuries to structures of the knee, including ligaments, cartilage or bone. The most common ligament injury is to the medial patellofemoral ligament (MPFL). Cartilage can be sheared off and occasionally small fractures occur.
Loose bodies (usually small fragments of cartilage or bone) can cause locking and catching of the knee, oftentimes causing additional cartilage damage. Nearly all first-time dislocations require an MRI to look for these associated injuries.

Non-Operative Treatment:
The initial treatment of a patellar dislocation is to use a brace. Bracing the joint will allow a decrease in swelling and pain, as well as an increase in stability. A physical therapy program is begun once the knee begins to heal. The exercises will help strengthen the thigh and buttock muscles to help keep the patella well aligned and stable.
Operative treatment:
If the dislocated patella does not heal properly or dislocation continues after non-surgical treatment, surgery may be recommended. Arthroscopic (minimally-invasive) knee surgery is typically used to remove loose bodies and treat other damage within the joint. The ligaments that hold the patella in place are reconstructed to hold the patella in the correct position. Occasionally, other procedures may be required to realign your joint and increase the stability of your patella.
Surgery for Patellar Instability / Dislocation
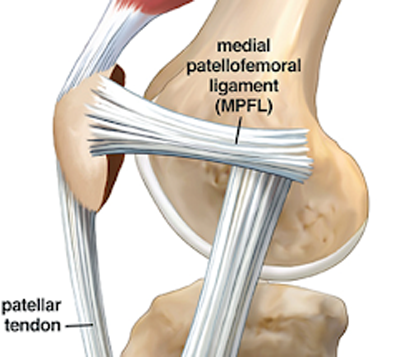
Anatomy: The most common reason for continued instability is a tear of the medial patellofemoral ligament (MPFL). This ligament is on the medial (inner aspect) of the knee that connects the patella (knee cap) to the medial femoral condyle (inner aspect of the thigh bone). The ligament is similar to a strong rubber band, in that it is elastic. The MPFL helps to stabilize the knee cap as it bends, and prevents the kneecap from dislocating to the outside of the knee. If the MPFL is torn, there is little preventing the patella from shifting laterally out of place.
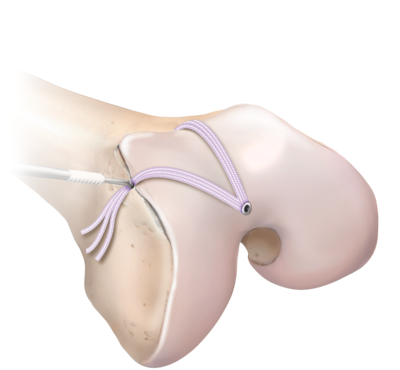
MPFL reconstruction: Surgery begins with an arthroscopy, where a small camera is inserted into the knee to look for damage to the cartilage and remove loose cartilage or bony pieces. The goal of surgery is to re-create the MPFL using an allograft (cadaver tendon). This allograft can be compared to a shoe-string. The two ends of the string are placed into two small holes in the patella (knee cap), while the looped end is secured into the femur (thigh bone) with a plastic screw. This is an outpatient surgery that is performed under general anesthesia. A nerve block is generally given before surgery to help with pain afterwards. You will be placed in a brace after surgery.
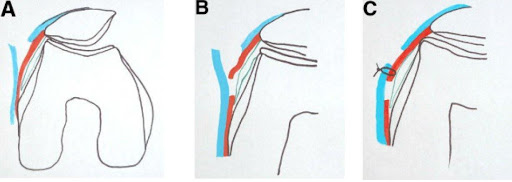
Open lateral retinacular lengthening: In some patients, the unstable kneecap is abnormally tilted. There are two layers of tissue under the skin (see blue and red lines in picture below) that attach to the kneecap and when tight, can cause the patella to sit off to the side. In these circumstances, an incision is made over the outer aspect of the knee. The layers are separated, lengthened and sewn back together to allow for the knee cap to sit in a more centered position in the trochlea (its groove).

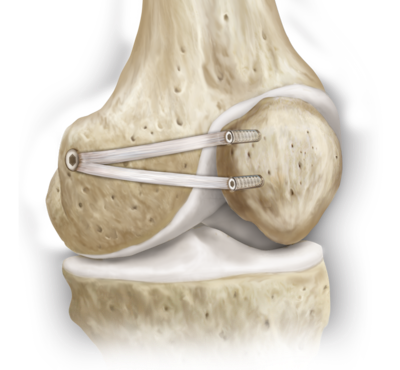
Osteochondral fracture fixation: Occasionally when the patella dislocates, it can shear off a piece of bone and cartilage. Significant swelling usually occurs. Surgery is recommended if there is a loose piece of bone/cartilage, even if it is a first-time dislocation. If the piece of bone attached to the cartilage is thin, it is usually removed. If there is enough bone to fix back to the patella, a larger open incision will be made and the fragment is repaired back to the patella with screws.

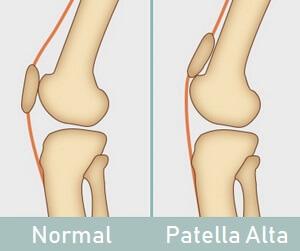
Tibial tubercle osteotomy: Rarely, the anatomy and angling of the tibia and femur can increase the risk of the patella dislocating. This can be due to the tibial tubercle (bony bump on the shin bone where the patellar tendon inserts) being located too far laterally (out to the side). An MRI determines the exact location. If the tibial tubercle is too far to the side, it must be shifted in surgery. This is performed with a large open incision over the front of the knee and is done at the same time as the MPFL reconstruction.
Trochleoplasty: In rare circumstances, the trochlea (groove in which the knee cap tracks) can be misshapen. The trochlea can be flat (your patella like an egg sitting on a table-top) or even humped (egg sitting on an egg). This surgery involves a large incision over the middle of the knee. The cartilage is lifted from the femur (thigh bone), and specialized instruments are used to reshape the trochlea to recreate a normal V-shape groove. This is a very complex procedure. There are significant risks and this procedure is reserved only for patients with severe abnormalities of the trochlea and/or failed previous MPFL reconstruction.
Patellofemoral Pain Syndrome
As the knee bends and straightens, the patella (knee cap) slides within a groove on the front of the femur (thigh bone) called the trochlea. The patella moves in many directions within this groove as the knee bends and twists to provide efficient, frictionless movement. The patella although mostly moves up and down, can also move side-to-side, rotate, and tilt. The surfaces of the patella and trochlea are covered with articular cartilage to make movement smooth. Repeated rubbing of the patella and trochlea stresses the joint and may even lead to a bone bruise. Sometimes the pain is caused by a weakening of the articular cartilage.
One or more of the following factors can lead to pain:
- Muscular weakness/tightness: A weakness or strength imbalance of the knee or hip muscles may alter the tracking of the patella. Tight muscles may also affect patellar tracking. The muscles and tendons of the knee and hip must be flexible, yet strong.
- Overuse: Repeated bending/straightening of the knee that occurs in activities such as running may lead to the disorder because of the increased pressure between the patella and femur when the knee is bent. A constant bending motion, especially on the weighted leg, for instance in squatting or lunging, can irritate the patella and cause a bone bruise to form.
- Alignment: The alignment between the hip and the knee (the Q angle) is thought to affect patellar tracking. Patients with a larger than normal Q angle (knock-kneed) may have more pain on the outside of the knee because of increased pressure on these areas. In particular, the Q angle of growing female athletes enlarges as the pelvis widens, increasing the risk for patellofemoral pain.
- Decreased patellar mobility: If the knee cap tightens, it can cause increased pressure on the surfaces, especially with bending. Isolated tightness laterally (outer aspect) can also cause abnormal tracking within the trochlea, again causing abnormal pressure points.
Non-operative treatment:
- Patellofemoral pain syndrome can almost always be effectively treated without surgery. It can take the knee six weeks or more to show improvement—often the same length of time the pain has been present, or occasionally longer.
- Physical therapy: Exercises focus on strengthening and rebalancing the muscles about the knee and hip. Occasionally a knee sleeve, splint, or taping may be recommended to support the joint.
- Activity modification: Physical activities should by decreased by at least 30% initially and should be limited to those with no or low impact, such as swimming or bicycling. Hyperflexion (knee bent greater than 90 degrees) activities should also be avoided. Exercises that cause pain should be avoided.
- Anti-inflammatory medication: over the counter Aleve or Ibuprofen may be used. Make sure to take this medication with a meal and a full glass of water. Discontinue if you are having an upset stomach or dark stools.
