Knee Cartilage Surgery in Indianapolis, IN and Mooresville, IN
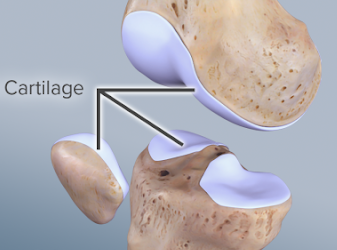
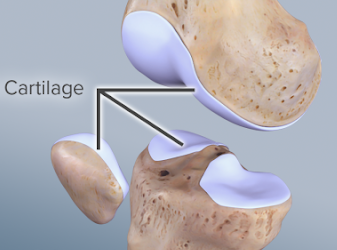
Cartilage Damage (Injury)

An articular cartilage injury, or chondral injury, may occur as a result of a pivot or twist on a bent knee, like the motion that can cause a meniscus tear. Damage may also be the result of a direct blow to the knee. Chondral injuries may accompany an injury to a ligament, such as the anterior cruciate ligament. Small pieces of the articular cartilage can actually break off and float around in the knee as loose bodies, causing locking, catching, and/or swelling. Oftentimes, there is no clear history of a single injury. The patient’s condition may, in fact, result from a series of minor injuries.
Non-Operative Treatment:
Articular cartilage damage that occurs over time is often treated without surgery. Some measures that the physician may recommend are:
- exercises to strengthen the muscles around the joint, sometimes including physical therapy
- changes in physical activity, including avoiding high impact (jumping, running) and knee hyper-flexion (knee bent past 90 degrees)
- weight loss
- shock absorbent shoe inserts
- Injections – may contain steroids, to help with the inflammation and pain, or hyaluronic acid, which help to lubricate the joint
- Medications – likely include nonsteroidal anti-inflammatories (Motrin, ibuprofen, Aleve, etc.) or analgesics (Tylenol, acetaminophen, tramadol, etc.)
Although there are many ways to treat the symptoms associated with articular cartilage damage, there are not any non-surgical options that can repair a cartilage injury or fill in a cartilage defect.
Any type of cartilage repair, if possible, requires surgery. In the past several years, there have been many exciting advances in the surgical treatment of articular cartilage defects. Factors that influence the choice of procedure include:
- size of the injury/defect
- location of the injury/defect in the knee
- age and weight of the patient
- patient’s future goals and activity level
- patient’s motivation and ability to participate in postoperative rehabilitation
- patient’s limb alignment: Is the patient bow-legged or knock-kneed?

Chondroplasty
This procedure uses special arthroscopic instruments (minimally-invasive) to smooth or remove the shredded, frayed or loose articular cartilage. It is a common treatment for patients with a cartilage injury that has not worn all the way down to the bone, especially under the kneecap. Ideally, this treatment will decrease friction and irritation, reducing the symptoms of swelling, noise (popping, clicking) and pain. This procedure is often done at the same time as other knee arthroscopic procedures like removing a torn portion of the meniscus (partial meniscectomy) or knee ligament procedures (ACL/MPFL).
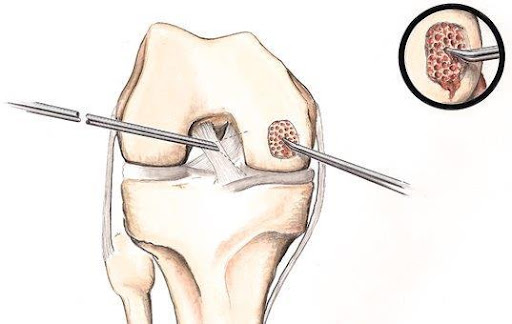
Microfracture
When damage involves the full thickness of the cartilage, small holes can be placed in the underlying bone. These tunnels allow the bone to “bleed” into the area of cartilage damage and form scar tissue. The scar tissue allows for less friction between the bones of the knee in comparison to injured cartilage. However, this type of scar tissue is not the same as the original cartilage of the knee. When microfracture is performed, you will be placed into a knee brace and on crutches with no weight allowed on the leg to let the scar tissue form and heal. This surgery is performed with an arthroscope (minimally-invasive camera) and is done as an outpatient with general anesthesia.

to use the patient’s own bone/cartilage. This technique is reserved for small areas of cartilage damage. After an open incision is made over the knee, the area of cartilage damage is removed. Using special instruments to match the exact size of the defect, a small plug of bone/cartilage is removed from an area of the patient’s knee where the bones do not contact one another. This plug is then transplanted into the original area of injury.
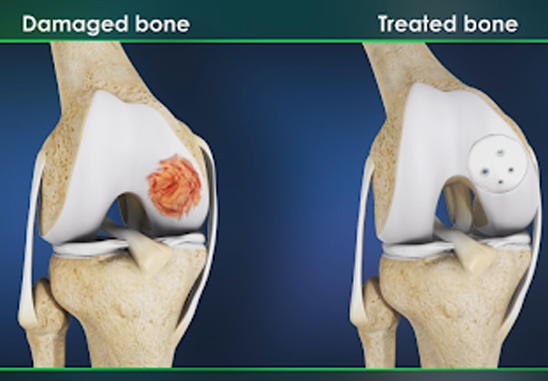
In larger areas of cartilage damage, there is an option to take a plug of bone and cartilage and place it into the defect. More commonly a cadaver (allograft) piece of cartilage/bone is used to fill in the defect. After an open incision is made over the knee, the area of cartilage damage is removed in its entirety and filled with the bone-cartilage plug.
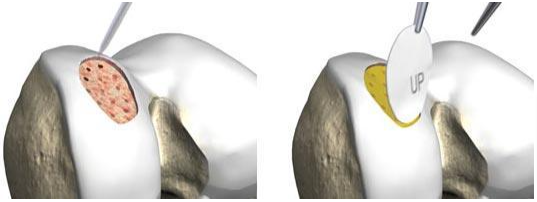
MACI is a procedure that requires 2 separate surgeries. First, healthy cartilage tissue is removed from a non-weightbearing area of the bone. This step is done as an arthroscopic procedure. The tissue, which contains healthy cartilage cells is then sent to the laboratory. The cells are cultured and increase in number over a 3- to 5-week period. The cells are placed onto a membrane in the laboratory. An open surgical procedure, or arthrotomy, is then done to implant the newly grown cells. The cartilage defect is prepared. The membrane with cartilage cells is then placed into the defect and glued in place and sealed with glue. MACI is most useful for younger patients. I prefer to use this technique in cartilage injuries involving the patella (kneecap). MACI has the advantage of using the patient’s own cells, so there is no danger of a patient rejecting the tissue.

In a certain subset of patients who require a surgery to correct cartilage damage, the leg is not completely straight. Patients can be in varus (bow-legged) or valgus (knock-kneed). If the limb is deemed to be out of alignment, an osteotomy may be performed. This involves an open incision over the femur (thigh bone) or tibia (shin bone). The bone is cut and shifted to allow the limb to straighten. This takes pressure off the area of the knee that is having the cartilage procedure and leads to better long-term outcomes.
Cartilage Damage (Degenerative)
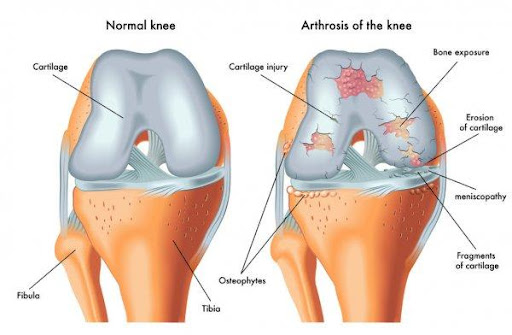

Non-Operative Treatment:
Goals are to decrease pain and improve function.
- Rest/Activity modification—your doctor may suggest avoiding squatting, kneeling and strenuous, high-impact activities like running and jumping.
- Non-steroidal anti-inflammatory medicines—drugs like ibuprofen and naproxen reduce pain and swelling. Make sure to take the medication with food to prevent stomach problems and with a full glass of water to prevent damage to the kidneys.
- Physical therapy—a physical therapist will initially focus on restoring normal motion to your knee. Stretching exercises to improve range of motion are very helpful, especially getting your knee straight. Once your pain has improved, your therapist can start you on a strengthening program for the supporting muscles that surround the knee and often include the hip.
- Steroid injection—if rest, activity modification, medications, and physical therapy do not relieve your pain, an injection of a local anesthetic and cortisone may be helpful. Cortisone is a very effective anti-inflammatory medicine that reduces pain and swelling.
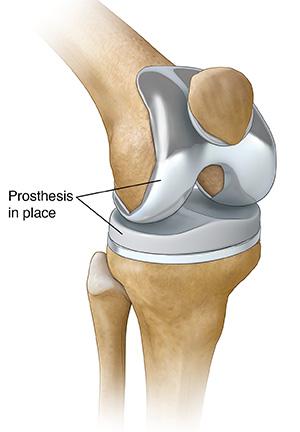
Operative treatment:
If the cartilage damage (severity of the arthritis) gets to a point where the above non-operative treatments are no longer helping, surgery is most often a total or partial knee replacement. Surgery to “clean up” the cartilage damage and/or arthritis very rarely helps with pain relief and overall function. If total joint replacement is recommended, I will refer you to one of my partners to discuss in greater detail.
