Shoulder Instability Treatment in Indianapolis, IN and Mooresville, IN
Shoulder Instability Information

Shoulder Instability
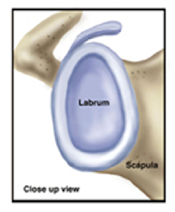
Shoulder instability describes a “loose” joint. The shoulder may have significant instability where the shoulder completely dislocates, or mild instability, where the shoulder is not firmly seated in the socket. There are two main types of instability – traumatic and atraumatic. Traumatic instability occurs after an injury or direct blow where the shoulder either completely dislocates and comes out of the joint, or nearly dislocates, also known as subluxation. The second type of instability is atraumatic. These patients suffer dislocations without any type of injury, and usually are born with loose joints. Generally, traumatic and atraumatic shoulder instability are treated differently.

Traumatic Shoulder Instability
Non-Operative Treatment: Initial treatment for instability of the shoulder centers on physical therapy. Strengthening the rotator cuff muscles and periscapular muscles (those around the scapula) gives stability to the joint. The goal of physical therapy is to help the muscles provide stability to the shoulder that the torn ligaments can no longer supply. The therapy for recurrent instability should be carefully designed for each patient since this condition often causes fear with certain arm positions or exercise moves. Very often, physical therapy can help regain lost motion, reduce apprehension, and restore shoulder function.
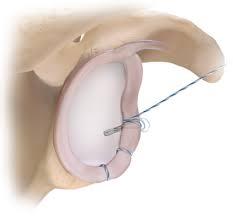
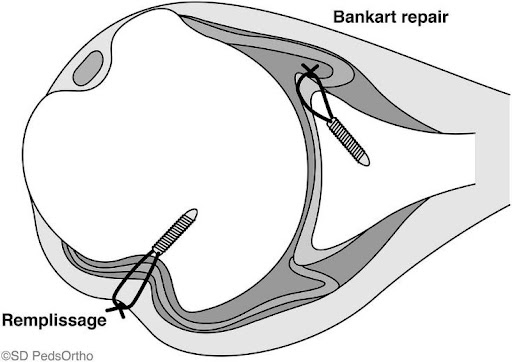
Surgery to repair the labrum is performed arthroscopically (minimally-invasive approach) with 3-4 small incisions in the skin. The torn labrum is fixed with anchors that go into the bone and have stitches that pull the labrum (bumper) back to the glenoid (socket). This is an outpatient procedure under general anesthesia. A pre-operative nerve block is given to help with pain after surgery.

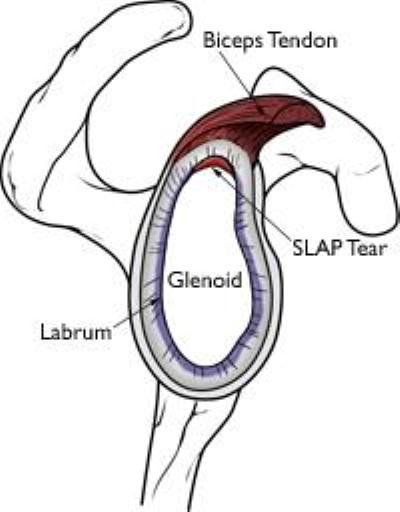
Labrum and Biceps-Anchor Complex Injury (SLAP tear)
Tears of the labrum can be the result of:
- A direct fall or blow to the arm resulting in abnormal or extreme motion of the humerus
- A forceful lifting maneuver
- Repetitive pinching of the humerus and attached rotator cuff on the posterior (back) labrum with the arm in an overhead and extended position. This injury is termed internal impingement (pinching of the soft tissues) and is most commonly seen in baseball and tennis athletes whose arms are frequently in overhead positions
A SLAP tear (“SLAP” is an acronym for superior labral anterior to posterior tear) is a very common labral injury that occurs on the top of the labrum, extending from the front to the back. This injury affects the attachment of the biceps tendon to the glenoid. An injury in this area can be extremely painful, as the biceps can repeatedly pull on the tear.
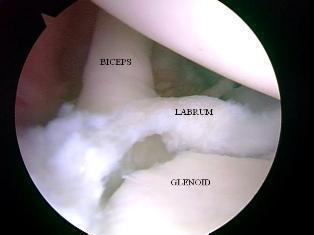
Tears that need treatment are usually seen when healing has not occurred. Tears involving the biceps tendon have more difficulty healing because the biceps constantly pulls on the labrum. Chronic tears may require surgery if patients are unwilling or unable to modify their activities sufficiently to allow for healing. Surgery should be considered if pain is unresponsive to: anti-inflammatory medications such as ibuprofen, rest, activity modification, physical therapy or if the labrum has not healed after an acute injury.
SLAP Tear Surgical Treatment

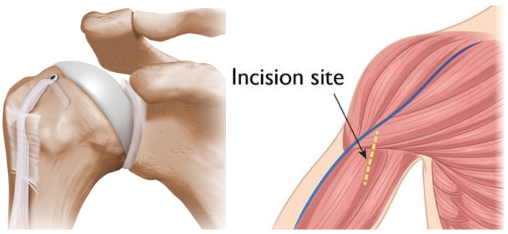
What Happens During Shoulder Ligament Reconstruction?
Shoulder ligament reconstruction surgery involves the repair of torn or stretched ligaments so that they are better able to hold the shoulder and collarbone in place. The surgery is performed as an open surgical procedure which involves one incision over the shoulder. This is an outpatient procedure done under general anesthesia. Most patients receive a pre-operative nerve block to help with pain after surgery.
Certain painful and unstable SLAP tears, in which the biceps is detached (separated from the glenoid/socket), need to be reattached to the bone. The surgeon uses anchors in the bone with stitches that fix the torn labrum back to the bone. This type of surgery is reserved for younger and highly active patients. Newer studies are showing that repair, as seen in the picture on the right, in older patients may limit motion too much and can hurt overall shoulder function.

Shoulder Multi-Directional Instability (MDI)
MDI patients often have increased ligament laxity in many joints. Hyperflexible knees, elbows, wrists, fingers and a self-described history of being “double-jointed” are common. These patients often have laxity in both shoulders. Because many athletes with MDI are quite successful in their sports, there is a debate about whether this type of laxity is harmful or can be helpful.
Most patients with MDI can be treated non-operatively with a physical therapy program that emphasizes muscular rehabilitation. There is a focus on strengthening the rotator cuff muscles and periscapular muscles (those around the scapula/shoulder blade). Building up these muscles provides improved stability to the joint. The vast majority of patients (about 90%) who follow a rehabilitation program diligently for at least six months will achieve stability and pain relief. Those who continue with a routine exercise program as outlined by the doctor are most likely to have a successful recovery. Athletes may also benefit from sport-specific rehabilitation that includes technique evaluation and modification. Often this type of program can help eliminate faulty practices that may have led to the instability, particularly with throwing athletes. The most challenging patient to treat surgically is the athlete whose symptoms continue following a rehabilitation program. Many athletes are successful in their sport because of increased laxity (movement) in the shoulder joint. Surgical intervention should only be considered when the patient has a thorough understanding of MDI, and is aware that stability with surgical correction is achieved at the expense of motion. Patients who have significant laxity, and can voluntarily dislocate their shoulder, tend to be poor surgical candidates. Surgery is rarely successful for them.
